CAR T-Cells For the Rest of Us

Last week, one of my co-bloggers (hi JG!) posted this article to the GP Facebook page. I was interested because the news of a one year old getting her leukemia cured is super exciting, but I was also intrigued because I work at a center that is conducting similar trials within my department. I’ve gotten quite the crash course on this type of treatment recently, so I thought it might be interesting to break the science down a little further for people who were interested.
Disclosure alert: I do work at and collect a paycheck from a medical center that is actively pursuing studies using technology similar to what I will discuss. Presumably someone I know would financially benefit somehow if this works well, and I’d have better job security. The articles and data I’m linking to however are not about my center, and I am writing this solely as a science enthusiast and not in a professional capacity.
With that out of the way, let’s get going!
Alright, first things first….how did we get here? What’s going on?
Okay, so let’s take a step back from the article and do a little overview of cancer care in general. As anyone who has ever had/loved/cared for/seen a person with cancer knows, chemotherapy and other cancer drugs can be beasts. They make you sick, they make you miserable, they work with broad strokes and many people really hate the treatments. They also don’t work for everyone, which is particularly awful. Given that, the goal of research has always been to 1) find something that would target cancer cells more specifically and 2) find something that works on more people.
There’s lots of ways to approach this of course, but one of the running ideas had been to modify a patients own cells and “hack” the immune system in to being able to kill of the cancer on it’s own. Broadly, it’s called “immunotherapy”.
Well that’s cool, but how do you do something like that?
Well, the first steps were to identify what cells we were trying to kill. For blood cancers (like leukemia), the key point was to look for a type of white blood cell called B cells. B Cells are the ones that produce antibodies, and they are also the types of cells that turn cancerous when someone gets leukemia. Luckily for us, B cells are pretty easy to identify and target by looking for a particular protein that they have on the surface of them called CD19. If you’re in to cell biology you can read more here, but basically all you need to know is that CD19 is an easy way to tell what’s a B Cell and what’s not.
That’s the easy part.
The hard part was figuring out how to get something to just seek out CD19 and destroy them all.
Okay, so how’d we do that?
Well, we targeted a different type of white blood cell, the T cell. On it’s own it’s not enough, but funny story. Sorta. It turns out we already kinda knew some things that were good at targeting immune system cells, so we just spliced them in and were on our way.
That was weirdly vague. What do you mean “we already kinda knew some things that were good at that”?
Well, um, what I meant to say, well, basically we used a virus. See some viruses are really good at attacking the immune system, so who better to call in for a consult?
Okay, that makes sense I guess, but you’re still being weird about this. What kind of virus did we use?
Okay, I’ll tell you. But you have to promise not to freak out,okay?
I PROMISE JUST TELL ME
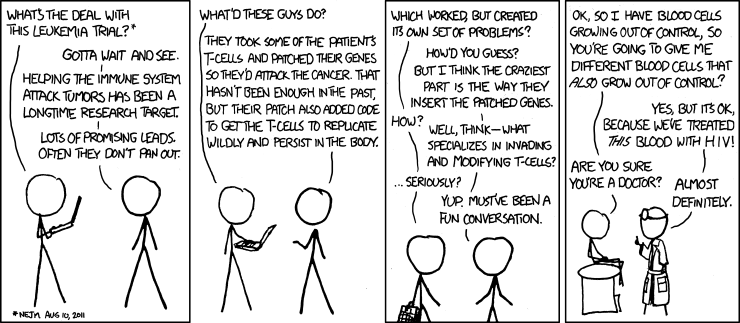
HIV. See, there was even an XKCD comic about it back in 2011:
You’re kidding, we’re using the scourge of humanity to try and fight the emperor of all maladies?
Yeah, kinda Alien vs Predator. I know. But I think this one might end well for us. It really makes sense if you think about it though….HIV is deadly because it takes out the parts of the immune system that typically would fight it off. If you can render the bad parts inert, it actually is pretty useful for something like this.
Okay, that’s cool I guess. So what are we calling this monstrosity?
CAR T cells. The “CAR” stands for “chimeric antigen receptor”. As a reminder, this is what the original chimera looked like:
Okay, so even scientists get this is a little crazy sounding?
Oh yeah. To be fair some of the studies currently going are looking at using different viruses or finding non-viral vector methods for doing this. It’s an active field right now.
So how’s this stuff worked out so far?
Pretty encouraging, but still early. The first attempts in humans were made in 2011, and the first guy to receive a version of these cells (featured in this article) is still alive almost 5 years later. For someone who had failed to respond to every other treatment, that’s pretty good.
After the first trial with kids this video was made:
https://www.youtube.com/watch?v=h6SzI2ZfPd4
That study, done exclusively on kids with acute lymphoblastic leukemia who had failed to respond to other types of treatment, found that 27 out of 30 kids responded to this. That’s a pretty good reason to get hopeful right there. Other trials have been similarly hopeful, with one in adults showing 5 out of 7 responding. Cancer.gov has compiled some more early results here.
The trials are still generally Phase 1 though, with a few moving in to Phase 2. Clinical trials-wise this means we’re actually just establishing general safety and only just starting to move in to larger recruitment goals.
So this has been going on for a couple years then….why did that little British girl make the news?
So there’s a couple unique things about her. First, the cells she got were not her own, but actually from a donor. That’s not too surprising. The really funky part is that the donor wasn’t matched to her, it was just a random donor. That’s unusual, because in the transplant world, you always have to match a donor. Some people don’t find one. It appears from the abstract here that this little girl didn’t have a perfectly matched donor, so the clinicians used some very new technology to render that irrelevant. This is the first time that’s been attempted in a human. To be clear, this was so early it wasn’t even part of a trial – it was a compassionate use case. Basically it was only allowed because there was no hope for her. They will now have to move on to a clinical trial. These results will be presented in a few weeks at the American Society for Hematology conference in Florida, and I’m sure we’ll hear more then.
So….what’s the down side? There’s always a downside, right?
Yeah, there’s always something. A few issues:
- The major side scary side effect is something call “cytokine release syndrome” which is very, very bad. All of the 30 kids on the study I mentioned above got it. It’s an extreme immune response where the body starts attacking itself, and it produces high fevers and can kill you. Future studies are looking at how to minimize this, but we’re not there yet.
- It’s still early, much is still unknown. My explanation above follows what the early studies did (and by early I mean 4 years ago), but there are lots of studies trying to tweak various aspects of those first trials to improve safety and get a better response. I did a quick search for ongoing trials sponsored by the National Cancer Institute using the phrase “CAR T”, and there are 49, all are Phase I or II. People are experimenting with types of cancer to target, dose to give, viral vector, and course of treatment. Given that many are likely multi-center trials, this is a huge investment in some very new technology. It could be years before this is sorted out and we know exactly how to use it best. Chances are good some of these trials will not pan out.
- The cost. At least currently, some of these therapies are being used as a bridge to bone marrow transplant. I poked around and some investors at economywatch.com are guessing that this therapy alone will run $250,000. A bone marrow transplant can easily cost the same amount or more, so even if this did work people would still be fighting with insurance companies over the cost. These are also incredibly resource intensive therapies, requiring well equipped processing labs, well trained staff, and other specialty resources. This means even if every single trial went perfectly, it could still be decades before we could even meet the demand, let alone find someone to pay for it. This is part of why the British study was exciting…creating an “off the shelf” product as opposed to one custom made for every patient could help the availability substantially.
- The hype. While it’s hard not to get excited when you see words like “cure” and “90% response rate”, it’s important to remember that tempered expectations lead to less disappointment. This could change everything, or it could become another weapon in the arsenal. Obviously people will work for the first, but the second option could still potentially help a lot of people.
- Long term effects. As long as we stay in early trials with people with no other options, the long term effects of these treatments are not terrifically relevant. As the reach expands however, and the first patients live longer, we may see some problems we haven’t considered yet. We do know that as long as these engineered cells are circulating, the patient will not have any of the cells they were designed to kill. In the case of the studies above, this means no B Cells and the immunity they normally bring. This can be fixed with periodic infusions of intravenous immunoglobulin, but the infusions have to be done for the rest of their lives….and that’s the best case scenario.
Whoa, that’s a lot to think about.
For sure. Keep your fingers crossed.





